🔍 Introduction
Microorganisms are so tiny that even with a light microscope, they cannot be seen clearly without proper staining. Staining adds contrast to otherwise transparent bacterial cells, allowing scientists to visualize their shape, arrangement, and internal structures.
In microbiology, staining techniques are not just about coloring cells — they are a gateway into the microbial world. By using different stains and dyes, researchers can:
- Differentiate between bacterial species,
- Identify pathogens in clinical samples,
- Highlight specific structures like spores and capsules,
- Classify bacteria for diagnosis and research.
Without staining, microbes would remain invisible and unclassified, limiting our understanding of their diversity and role in health, disease, and the environment.
🎨 Types of Staining Methods in Microbiology
Different staining techniques are used depending on the purpose of study. Here are the most important methods:
1. Simple Stain
- Principle: Uses a single basic dye (e.g., methylene blue, crystal violet, safranin).
- Purpose: Enhances visibility of bacterial cells to study size, shape, and arrangement.
- Example: Observing cocci (spherical) and bacilli (rod-shaped) bacteria.
✅ Advantage: Quick, easy, and ideal for beginners.
❌ Limitation: Does not differentiate between bacterial species.
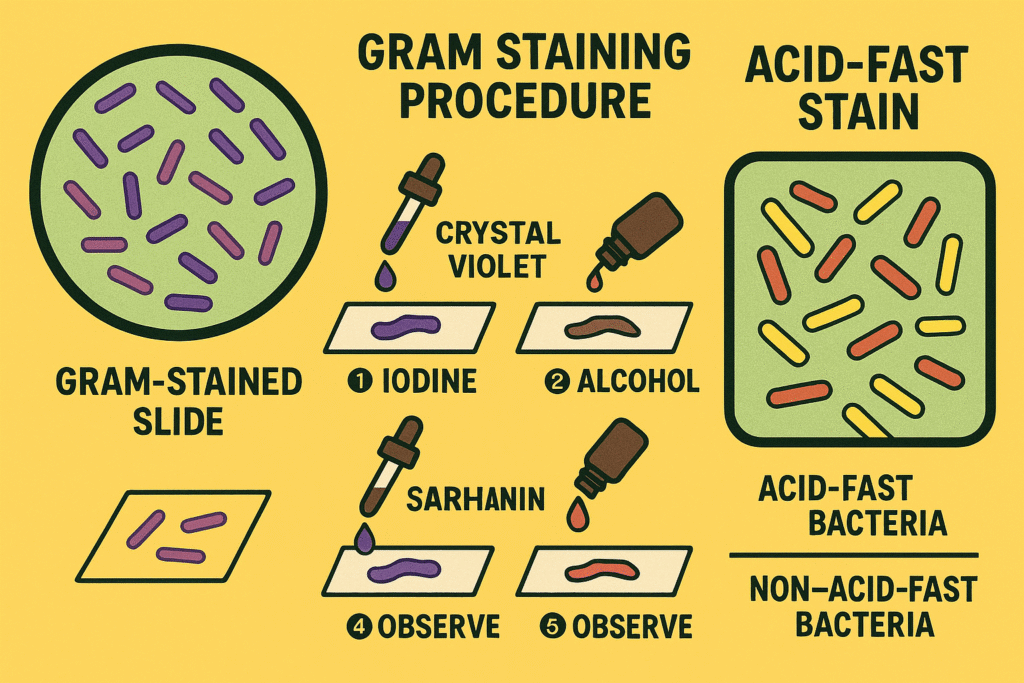
2. Gram Stain (Differential Stain)
- Developed by: Hans Christian Gram (1884).
- Principle: Differentiates bacteria based on the structure of their cell walls.
- Procedure Steps:
- Primary stain (Crystal violet)
- Mordant (Iodine)
- Decolorizer (Alcohol/Acetone)
- Counterstain (Safranin)
- Results:
- Gram-positive bacteria: Purple (thick peptidoglycan layer retains dye).
- Gram-negative bacteria: Pink (thin peptidoglycan layer, dye washes out).
- Uses: First step in bacterial identification, clinical diagnosis, and antibiotic selection.
✅ Advantage: Widely used, provides key classification.
❌ Limitation: Some bacteria (e.g., Mycobacterium) do not respond well.
3. Acid-Fast Stain
- Principle: Detects bacteria with waxy mycolic acid in their cell walls (e.g., Mycobacterium tuberculosis).
- Stains Used:
- Primary stain: Carbol fuchsin (red)
- Decolorizer: Acid-alcohol
- Counterstain: Methylene blue
- Results:
- Acid-fast bacteria: Retain red color
- Non–acid-fast bacteria: Appear blue
- Clinical Use: Essential for diagnosing tuberculosis and leprosy.
4. Endospore Stain (Schaeffer–Fulton Method)
- Principle: Highlights bacterial spores, which are resistant to heat, radiation, and chemicals.
- Stains Used:
- Malachite green (stains spores)
- Safranin (stains vegetative cells)
- Results:
- Spores = Green
- Vegetative cells = Red/Pink
- Use: Identifying Bacillus and Clostridium species (e.g., anthrax, tetanus).
5. Negative Stain
- Principle: Instead of staining the cells, the background is stained using acidic dyes (e.g., nigrosin, India ink).
- Purpose: Visualizes cell shape and capsules without heat fixation.
- Result: Cells appear clear against a dark background.
✅ Advantage: Preserves natural morphology.
❌ Limitation: Less permanent; slides may fade.
6. Capsule Stain (Optional Advanced Method)
- Principle: Detects capsules, which are protective layers around certain bacteria (e.g., Klebsiella, Streptococcus pneumoniae).
- Method: Combination of negative staining (background) and simple stain (cell body).
- Result: Capsule appears as a halo around the cell.
🧠 Applications of Staining in Microbiology
Staining techniques are indispensable in microbiology for:
- Identifying Bacteria in Clinical Samples
- Doctors rely on stains like Gram stain and Acid-fast stain for quick diagnosis.
- Helps in selecting appropriate antibiotics.
- Studying Cell Structures
- Detecting spores, flagella, capsules, and nuclei.
- Understanding bacterial defense mechanisms.
- Differentiating Pathogenic vs. Non-Pathogenic Microbes
- Gram-negative bacteria are often more pathogenic due to endotoxins.
- Acid-fast staining confirms serious infections like TB.
- Educational and Research Purposes
- Teaching basic microbiology.
- Classifying unknown microorganisms.
🧪 Best Practices for Effective Staining
- Always prepare fresh smears on clean, grease-free slides.
- Use the correct concentration and timing for stains.
- Do not overheat during heat fixation; it may distort cells.
- Wash excess stain gently to avoid losing the smear.
- Observe slides under oil immersion objective (100x) for best clarity.
✅ Conclusion
Staining techniques are truly the window to the microbial world. Without them, bacteria would remain invisible, making diagnosis, research, and classification impossible.
From a simple stain that highlights basic cell shapes to advanced methods like Gram staining, Acid-fast staining, and Endospore staining, these techniques are the foundation of microbiology laboratories.
By learning and practicing these methods, microbiologists can accurately identify organisms, study their structures, and contribute to better healthcare and scientific discovery.